Mental Health – Part 2: Mechanisms of Disease
See Part 1
Mental health vs Neurologic health
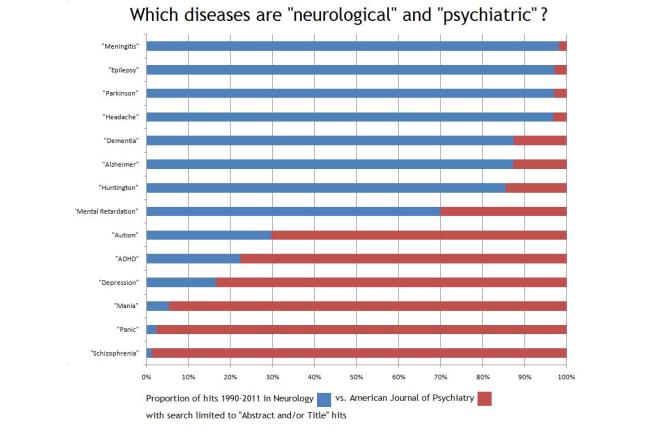
Historically, there has been a divide between the medical fields of Neurology and Psychiatry, despite some overlap between the two specialties. Dementia is predominantly under the jurisdiction of neurology, as are seizures/epilepsy, headaches, movement disorders, and multiple sclerosis. Mental health disorders, however, are categorized in the field of psychiatry, including mood disorders, ADHD, autism, and psychosis.
Given the many similarities among these conditions in terms of the underlying causes and their response to certain treatment approaches, it may be more useful to look at these neurologic conditions and psychiatric conditions under a collective category of “brain health”. Let’s explore some of the factors that contribute to problems with brain health.
Mechanisms of brain dysfunction
Many psychiatric disorders share common pathologic mechanisms, meaning that the same biochemical processes appear to be driving disease in each of these conditions. Some of these same mechanisms have also been demonstrated in neurologic diseases.

- Decreased cerebral glucose metabolism. The brain has difficulty using glucose as an energy source in certain conditions, including Alzheimer’s, Parkinson’s Disease, epilepsy, depression, bipolar disorder, and schizophrenia. There is autopsy evidence of decreased glucose transporters and increased ketone importers in the schizophrenic brain.
- Imbalance of neurotransmitters. The relative amounts of the chemical messengers in the brain appear to be relevant to many brain conditions, including dopamine, serotonin, GABA, and glutamate.
- Oxidative stress. Certain chemicals are unstable and create free radicals, or reactive oxygen species. In a pathological state, our antioxidant defenses are not robust enough to protect us from this damage, which can result in damage to nucleic acids (DNA and RNA), proteins, and lipid membranes. This form of chemical stress appears to contribute to all chronic diseases.
- Inflammation. There is evidence of increased inflammatory markers in the brain in depression, bipolar disorder, and schizophrenia, indicating the presence of inflammation.
- Gut microbiome. The gastrointestinal tract
 is intimately controlled by the nervous system, and there is likely 2-way communication between the gut and the brain via an abundant network of nerves. Dietary factors affect the microbiome of the gut which may alter absorption of nutrients, weaken the intestine’s barrier against toxins, and be subject to inflammation. These processes may have negative consequences to the central nervous system.
is intimately controlled by the nervous system, and there is likely 2-way communication between the gut and the brain via an abundant network of nerves. Dietary factors affect the microbiome of the gut which may alter absorption of nutrients, weaken the intestine’s barrier against toxins, and be subject to inflammation. These processes may have negative consequences to the central nervous system.
With similar processes at play in these disorders typically categorized in either neurology or psychiatry, it may be more fitting to refer to them as neurometabolic diseases.
We have a processed food problem
These mechanisms of injury to the brain likely have a common thread: they are all caused by the consumption of processed foods. Since the mid-20th Century, there has been exponential growth of the processed food industry in the United States,
- Of 230,156 packaged food and beverage products examined in one study, 71% of the products were classified as ‘ultra-processed’. Of the products produced by the top 25 manufacturers (by sales volume) of packaged foods, 86% of the items were classified as ‘ultra-processed’.
There is increasing recognition of the unfortunate health consequences of processed food consumption and the role that they play in chronic disease.
Ultra-processed foods are associated with mental disorders, such as depression. In addition, ultra-processed foods are associated with metabolic dysfunction which, in turn, is another driver of depression.
The ingredients commonly found in ultra-processed foods are sugar, refined grains, and seed oils. There is clear evidence that sugar-sweetened beverages increase inflammation. Seed oils also contribute to inflammation due to their Omega-6 fatty acid content.
Connections to metabolic health
Mental health disorders  are associated with impaired metabolic health – metabolic syndrome, diabetes, cardiovascular disease, etc. While many medications used for these conditions are associated with weight gain and worsened glucose tolerance, this finding is consistent among individuals receiving all sorts of treatments and even those who have not received treatment. Also, despite the association of mental health disorders with poor lifestyle and drug use, the association with metabolic disease is present even among healthy weight and drug-naïve patients.
are associated with impaired metabolic health – metabolic syndrome, diabetes, cardiovascular disease, etc. While many medications used for these conditions are associated with weight gain and worsened glucose tolerance, this finding is consistent among individuals receiving all sorts of treatments and even those who have not received treatment. Also, despite the association of mental health disorders with poor lifestyle and drug use, the association with metabolic disease is present even among healthy weight and drug-naïve patients.
Neurometabolic diseases are driven by complex but similar mechanisms, which may explain why some medications are used to treat disorders that are seemingly quite different, e.g. valproic acid for seizures (epilepsy) and for mania (bipolar disorder), and are prescribed routinely by both neurologists and psychiatrists. Perhaps thinking of these disorders in terms of overall brain health and acknowledging the important role of metabolic health will allow for a more effective approach in the future.