Can Low Carb Help Lung Disease?
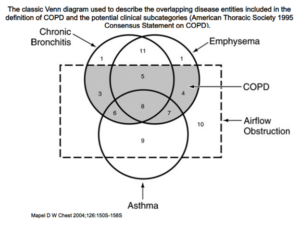
The two most common chronic lung diseases are asthma and COPD. It’s estimated that at least 384 million people across the globe have COPD and 334 million people have asthma. COPD is now the third leading cause of death worldwide.
While smoking is the main cause of COPD in the United States, studies estimate that 24% of those with COPD have never smoked. In these cases, the causes for COPD may include occupational exposure and genetic conditions.
Individuals with asthma and COPD are at risk for acute exacerbations, or flare-ups, of their chronic lung disease. Occasionally these flare-ups are severe enough to require hospitalization. COPD exacerbations, which are most commonly triggered by infection and exposure to irritants, rank among the top reasons for hospitalization.
Asthma occurs in lungs that have a heightened immune response to environmental stimuli leading to inflammation and increased sensitivity of the airway. This inflammation leads to the characteristic “wheeze.” Asthma is typically approached by reducing environmental triggers, using inhaled steroids that treat the inflammation, and inhaled bronchodilators (broncho = airway, dilator = relax) that cause the smooth muscle in the airways to relax.
COPD or “chronic obstructive airway disease,” is also caused by inflammation in the airways; however, unlike asthma, the obstruction does not resolve completely with bronchodilators. COPD leads to scarring of the small airways and destruction of the alveoli (the small “balloons” where the lungs exchange oxygen and carbon dioxide). The treatment of COPD relies heavily on smoking cessation, avoidance of other environmental triggers, and using inhaled steroids as well as bronchodilators.
- Diet and lung function
Modern medicine offers us a variety of interventions that target specific disease mechanisms. In the case of lung diseases such as asthma and chronic obstructive pulmonary disease (COPD), the primary targets of drugs are inflammation and bronchodilation (relaxing of the airways).
Although inflammation is indeed a key player in acute episodes of COPD and asthma, there are other relevant mechanisms current treatments do not target and perhaps many more that we have yet to discover. (ref)
The most beneficial intervention for COPD is to abstain from smoking. Medical therapy with inhaled steroids and bronchodilators is aimed at improving quality of life, as well as reducing exacerbations and hospitalizations; however, it unfortunately does not change the natural course of the disease or prolong survival. (ref)
Similarly, asthma is treated mainly with bronchodilators and steroids, and patients are told to control their exposure to allergens or irritants that may worsen asthma symptoms.
However, the role of nutrition in managing lung disease has not been well-researched or emphasized in education, despite the fact that these patients face some significant nutritional challenges.
For example, one issue for patients with COPD is loss of muscle and fat mass due to a complex process called pulmonary cachexia. (ref) Current nutrition guidelines for COPD focus primarily on correcting malnutrition and providing adequate energy intake to prevent weight loss. (ref)
Even in the absence of respiratory disease, malnutrition causes decreased respiratory muscle mass and function, a problem with more significant implications in those with chronic lung disease. (ref)
According to the Academy of Nutrition and Dietetics, macronutrient advice should be based on a patient’s preference, because there is limited evidence for recommending any specific macronutrient composition. (ref)
Despite a lack of formal recommendations, however, some lung disease specialists (pulmonologists) have recognized the utility of low carb, ketogenic diets in COPD. Dr. Albert Rizzo, MD, the chief medical officer of the American Lung Association, acknowledges the potential benefit of the ketogenic diet in COPD, citing anecdotal evidence: “Some notice they can walk faster and climb steps easier.”
Dr. Raymond Casciari, MD, another pulmonologist, states: “If you eat a high-carbohydrate diet and you have COPD, you will wind up more short of breath … The best kind of diet for a person with COPD is a high-fat, high-protein, low carb eating plan like the keto diet.”
In the following sections of this guide, we will explore the mechanisms by which carbohydrate reduction could play a therapeutic role in the treatment of lung disease:
- Reducing body weight in patients with obesity
- Reducing inflammation
- Reducing high blood sugars
- Reducing carbon dioxide production
- Improving nutrition density of meals
- Lung disease, diet, and inflammation
Doctors understand that both asthma and COPD are defined by inflammation of the airways (ref, ref, ref). Inflammation results in mucus production, coughing, shortness of breath, and wheezing.
Depending on the severity of the exacerbation, patients may require breathing treatments that help open the airways (bronchodilators), antibiotics, steroids, supplemental oxygen, and even hospitalization.
Carbohydrate restriction reduces inflammation
Given that COPD and asthma are driven by inflammation, any intervention that reduces inflammation could theoretically have a beneficial effect on these chronic lung diseases.
Low carbohydrate diets, compared to low fat diets, can result in reduced markers of inflammation for many individuals and thus may be useful in lung disease. (ref)
Nutritional ketosis suppresses the NLRP3 Inflammasome
The NLRP3 inflammasome  is a cellular inflammatory complex implicated in COPD exacerbations and has been shown to be triggered by infections, cigarette smoke, and air pollutants. It is thought to be involved with the development and progression of COPD and to play a significant role in acute exacerbations. (ref)
is a cellular inflammatory complex implicated in COPD exacerbations and has been shown to be triggered by infections, cigarette smoke, and air pollutants. It is thought to be involved with the development and progression of COPD and to play a significant role in acute exacerbations. (ref)
The ketone body beta-hydroxybutyrate suppresses the activation of the NLRP3 inflammasome. (ref, ref) The clinical significance of this suppression of inflammation is unknown at this time but is a potentially promising feature in the role of the ketogenic diet as a treatment for COPD.
- High blood glucose and lung disease
Hyperglycemia (high blood glucose level) is common during lung disease exacerbations, both as a response to stress and as a side effect of medical management.
Because they reduce inflammation, steroids (glucocorticoids) are a standard part of treatment when a patient has a COPD exacerbation. One study estimated, however, that 45% of individuals treated with steroids for COPD exacerbations develop steroid-induced diabetes. (ref)
Even those hospitalized patients who do not meet criteria for steroid-induced diabetes will often develop higher-than-normal blood sugars when receiving high-dose corticosteroids (prednisone greater than or equal to 40 mg daily).
Hyperglycemia is associated with adverse outcomes
Just as type 2 diabetes is associated with worsened outcomes in many other medical conditions, hyperglycemia is associated with poor outcomes in patients admitted to the hospital with acute exacerbations of COPD. (ref, ref)
Pre-existing hyperglycemia also makes these patients more prone to exacerbations of their lung disease. (ref) Not only is hyperglycemia relevant in the setting of exacerbations, but long-standing hyperglycemia also has a significant impact on the long-term course of lung disease:
- Type 2 diabetes is associated with worsening progression of COPD and increased COPD-related mortality. (ref, ref)
- Results of pulmonary function tests are decreased in those with type 2 diabetes compared to healthy controls. (ref)
- For individuals with COPD, higher fasting glucose (as seen in metabolic syndrome) is associated with increased frequency of exacerbations. (ref)
- People with type 2 diabetes are more likely to have reduced pulmonary function, reduced exercise capacity, and reduced quality of life compared to people without diabetes. (ref)
- When patients with diabetes and COPD are hospitalized for an exacerbation, 50 – 80% of them experience high blood glucose, have longer hospital stays, and increased mortality compared to patients without diabetes. (ref)
Hyperglycemia disrupts airway glucose regulation
Glucose levels in the airway are typically regulated to keep levels low; however, inflammation as well as high blood glucose disrupts this regulation and leads to increased levels of glucose in the airway. (ref) Glucose in the airways serves as a nutrient source for bacteria, which can contribute to infections and exacerbations of chronic lung disease.
Metformin, a medication that reduces hyperglycemia, is associated with reduced bacterial growth in the airways. In one observational study, patients with asthma and diabetes who took metformin had a five-fold lower risk of asthma-related hospitalization and two-to three-fold lower risk of asthma exacerbations. (ref)
Carbohydrate reduction reduces hyperglycemia
Carbohydrate reduction improves blood glucose in patients with type 2 diabetes. (ref)
It is plausible that low carbohydrate diets (which lower blood glucose and inflammation) would also lower glucose in the airway, reduce bacterial infections, and thus reduce exacerbations. Since improving overall glycemic control is associated with improved outcomes in both chronic and acute lung disease, a low carb diet has the potential to improve the clinical course of lung disease.
- Diet and carbon dioxide production
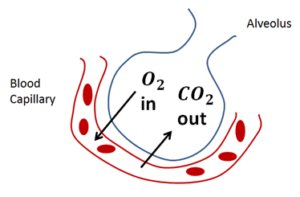
In simple terms, the lungs are responsible for ventilation — bringing oxygen into the body and removing carbon dioxide from the body.
Macronutrient intake affects carbon dioxide production
The amount of carbon dioxide produced from food differs depending on whether the food is made up predominantly of carbohydrate, protein, or fat. We measure this by comparing how much carbon dioxide is produced relative to oxygen consumed when food is being metabolized. (ref)
Respiratory Quotient
This ratio of oxygen consumed to carbon dioxide produced is called the respiratory quotient (RQ).
Carbohydrate produces the most carbon dioxide and has the largest RQ of 1.0. The RQ for fat, however, is only 0.7, indicating that less carbon dioxide is produced from eating fat. Protein falls somewhere between those two, with an RQ of 0.8.
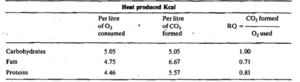
Why is this RQ value important? Because the body must get rid of the carbon dioxide it produces. As more carbon dioxide is created by the burning of fuel inside our bodies, our lungs need to work harder to blow off the carbon dioxide that accumulates.
 When you burn carbohydrates, there is more carbon dioxide which is like smoke from a fire. It will thus take more ventilation to remove the smoke from the air. In contrast, burning fat produces less smoke (carbon dioxide) and therefore does not require as much ventilation.
When you burn carbohydrates, there is more carbon dioxide which is like smoke from a fire. It will thus take more ventilation to remove the smoke from the air. In contrast, burning fat produces less smoke (carbon dioxide) and therefore does not require as much ventilation.
Healthy lungs can easily compensate for higher carbon dioxide production by increasing ventilation. However, those with COPD have impaired ventilation and may therefore develop high levels of carbon dioxide in the blood (a potentially dangerous condition called hypercapnia).
Thus, it may be favorable to reduce carbohydrate intake and increase fat intake to reduce production of carbon dioxide. The less carbon dioxide that is produced, the less effort it takes to get rid of it.
Carbohydrate restriction improves ventilation in COPD
The concept that low carb diets are better tolerated in individuals with chronic lung disease is not just a mechanistic theory. Studies support it as well.
A randomized, double-blinded study in a metabolic unit compared the effects of diet over the course of five days. (ref) Investigators randomly gave COPD patients diets consisting of low-, moderate-, and high-carbohydrate content (28, 53, and 74 percent carbohydrate, respectively) and measured the effects on respiratory function.
Subjects on a low carb diet produced less carbon dioxide and had lower levels of carbon dioxide in the blood compared to those consuming higher-carbohydrate diets. After only two weeks on a low carbohydrate diet, patients also had a significant 22 percent improvement in their lung function.
Whether carbohydrate restriction results in decreased morbidity and mortality from COPD is not yet known. However, even small improvements in ventilation in patients with COPD from a low carb diet may be clinically relevant for those who are at risk for respiratory failure.
- Low carb diets and the mechanics of breathing
For individuals with lung disease, there are additional benefits of carbohydrate restriction related to the work of breathing.
In the setting of an exacerbation of lung disease, breathing suddenly becomes the number one priority. Patients in respiratory distress often don’t feel hungry, may be too lethargic to eat, or may have mechanical barriers to eating, such as an oxygen mask or BiPAP mask in place.
Their situation may be so delicate that even temporary removal of the mask would be risky. Smaller, more nutritious meals may be preferable in order to meet the patient’s energy needs and allow sufficient rest between meals. (ref)
Carbohydrate-restricted diets focus on providing essential nutrients, especially protein, which is particularly important when patients are recovering from an illness.
Patients whose food intake is limited also need energy-dense foods, and fat provides more than twice as much energy per gram as carbohydrate, without raising blood sugar levels. Thus, a carbohydrate-restricted diet could supply smaller-volume meals with increased calorie and nutrient density. This could be important when every bite matters.
- Evidence: diet and asthma
In 1930, researchers selected 15 children (ages 3-15 years) with severe, chronic asthma who did not respond to conventional treatment for a trial of a low carbohydrate, ketogenic diet. (ref)
At the end of the third week, 14 of 15 children showed moderate or marked improvement in their asthma. These improvements were maintained for two months, and several children continued to participate with moderate to marked improvement for up to 10 months.
While this study showed promise, there has not been subsequent published research on the role of low carbohydrate diets in asthma.
There is, however, a randomized controlled trial that compared a Mediterranean diet that included fatty fish consumed twice weekly (intervention) with the usual diet (control) in children with mild asthma. Children in the intervention group were found to have decreased bronchial inflammation and decreased medication use. (ref)
This paper shows that diet quality matters and can have an impact on the lives of patients living with asthma.
- Evidence: high fat supplemental feeding in critical care
Individuals who suffer severe or complex lung disease may require mechanical ventilation in a critical care setting, such as the intensive care unit.
Since these patients are intubated (in other words, they have a tube inserted in the airway) and usually sedated, they are not able to eat and instead are given tube feedings (liquid nutrition delivered into the stomach) or total parenteral nutrition (TPN), which is delivered through the veins.
In trials of critically ill patients, tube feeding with a low carb, high-fat solution was superior to standard, high-carbohydrate formulas, as measured by a lower carbon dioxide concentration in the blood and a significantly shorter duration of mechanical ventilation.
In fact, the high-fat group spent an average of 62 hours less on the ventilator in two separate studies. (ref, ref)
TPN formulas that are mostly glucose are associated with significant increases in carbon dioxide production and increased respiratory effort to remove it, compared to formulas that contain a higher percentage of fat. (ref, ref)
There are even published case reports of individuals developing respiratory failure within hours after being started on high-carbohydrate TPN. (ref) It is theorized that the large carbohydrate load increased carbon dioxide production, which led to the rapid respiratory failure.
- Evidence: use of supplements in COPD
Nutrition supplements are a standard intervention utilized by dietitians to correct malnutrition in patients, as supplements are calorie-dense and easy to consume. It is important to consider that the macronutrient composition of supplemental meals likely matters.
One study showed that standard high-carbohydrate supplements caused an increase in carbon dioxide load and a decrease in exercise tolerance compared to lower-carb, higher-fat supplements with the same caloric content. (ref) Another study has shown that use of high-fat supplements is associated with improved lung function in patients with COPD. (ref)
A review of supplementation with specific nutrients showed that a variety of dietary interventions are associated with improvements in COPD patients: (ref)
- omega-3 fatty acids are associated with decreased inflammatory markers
- essential amino acids are associated with increased lean body mass, strength, and cognitive function
- vitamin D is associated with a reduced risk of COPD exacerbations
- antioxidant vitamins, selenium, calcium, chloride, and iron are independently associated with a higher volume of air that can be forced out in one second after taking a deep breath (called “forced expiratory volume in 1 second” or FEV1)
While it’s difficult to draw conclusions from correlational studies, due to confounding variables, it seems likely that one’s dietary pattern will impact outcomes.
Perhaps the most important takeaway regarding supplements is that high-fat supplements are an option to correct malnutrition without causing potential negative respiratory side effects that have been identified with standard, high-carb supplements.
- Conclusion
There is a dynamic relationship between metabolic disease and chronic lung disease in which one can exacerbate the other. Improving metabolic disease with nutrition may provide benefit in altering the natural history of chronic lung disease.
A low carb dietary intervention may be an important, under-utilized tool in treating asthma and COPD due to its beneficial effects on glycemic control, carbon dioxide production, and inflammation. Moreover, it is nutrient-dense and therefore may improve the nutritional status of those with advanced COPD.
Numerous studies have documented the effects of low carb diets improving lung function in patients with lung disease, both in acute and chronic disease states. In addition, the anti-inflammatory and glucose-lowering effects of eating low carbohydrate diets have been well-documented. This could translate into fewer bacterial infections in the lungs, fewer exacerbations, and improved outcomes.
For patients with limited ventilatory reserve, even a small improvement in lung function may be clinically relevant. Therefore, for patients who are in a borderline situation and at risk for respiratory failure, the advantages that come with a low carb diet may be particularly meaningful.
These advantages over the standard approach to managing lung disease make low carb diets a potential powerful adjuvant therapy for individuals with lung disease. Future high-quality studies would help explore the efficacy of low carbohydrate diets for asthma and COPD to improve care and shift medical practice.
[i] Lung function is measured by breathing into a device called a spirometer. One measurement is called Forced Vital Capacity (FVC), which measures the total amount of air that a person can exhale. Another measurement is called Forced Expiratory Volume 1 (FEV1), which is the amount of air a person can exhale in one second. In this study both the FEV1 and FVC improved by more than 20 percent indicating a marked improvement in obstructive airway disease.